
To kick off IBS Awareness Month this April, we partnered with Registered Nutritional Therapist and founder of Gutfulness Nutrition Gut Health and IBS Expert, Marilia Chamon, to answer her most frequently asked questions around IBS from her clients and followers.

1. What is Irritable Bowel Syndrome (IBS)?
IBS is a disorder of the gut-brain axis characterised by a collection of symptoms that include abdominal pain, bloating, cramping, gas, diarrhoea, and constipation. These symptoms can vary in severity and duration and can be triggered by stress, certain foods, hormonal changes, or other factors. It is estimated that IBS affects 1 in every 5 people in the UK.
2. What causes IBS?
One of the most common known causes of IBS is food poisoning, or catching a stomach bug, but other factors can contribute to its development too. Other causes of IBS can include:
- Altered gut motility
- Inflammation
- Changes in the gut microbiome
- Heightened gut sensitivity (also known as visceral hypersensitivity)
3. Can IBS be cured?
At present, IBS is considered a chronic condition and can’t be cured. It is important to highlight that other conditions can mimic IBS symptoms and should be ruled out before a final IBS diagnosis. Inflammatory bowel disease and Coeliac diseases are often the two conditions ruled our prior to an IBS diagnosis, however a recent systematic review and meta-analysis looked into the misdiagnosis of IBS and concluded that treatable gastrointestinal conditions such as small intestinal bacterial overgrowth (SIBO), lactose malabsorption, fructose malabsorption, bile acid diarrhoea, pancreatic insufficiency and microscopic colitis can be found in a proportion of individuals with IBS-like symptoms.
4. Why am I always bloated even though I eat a healthy diet?
There’s no one set answer to ‘why am I always bloated?’, but it may be due to something known as FODMAPs.
It may sound controversial, but some of the healthiest foods can sometimes be a trigger for IBS symptoms, especially if you have a sensitive gut. Foods high in FODMAPS (a collection of short chain carbohydrates and sugar alcohols naturally found in foods) are poorly absorbed in the small intestine and when they pass through to the large intestine, they are fermented by gut bacteria, resulting in gas production.
FODMAPs are also highly osmotic, meaning they attract water into the large intestine, which can alter how quickly bowels move. Those processes can result in symptoms such as excess wind, abdominal bloating and distension, and abdominal pain. Symptoms can also include constipation and diarrhoea, or a combination of both. Working with a FODMAP-trained nutritionist is advised so you can identify your triggers and tailor a diet specific to your needs.
5. Should I take a probiotic supplement?
Some individuals may benefit from probiotics for IBS, but there’s no one-size-fits-all solution to managing symptoms. When choosing a probiotic supplement for IBS, it’s important to choose a high-quality product containing strains that have been clinically studied for their effectiveness in IBS symptoms.
The effects of some strains of probiotics for IBS have been studied for their potential benefits, including the following (but not limited to):
- Bifidobacterium breve, Bifidobacterium longum, or Lactobacillus acidophilus significantly reduced abdominal pain
- Bifidobacterium breve, Bifidobacterium infantis, Lactobacillus casein or Lactobacillus plantarum significantly reduced abdominal distention
Aguulp Daily Synbiotic:
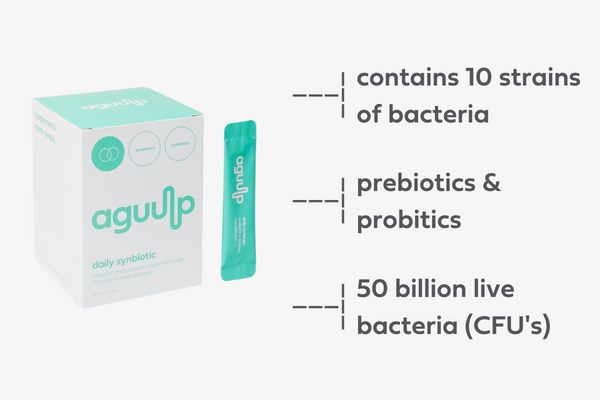
Aguulp Daily Synbiotic is a high-quality supplement which contains both pre and probiotics in a high dose, which are designed to work synergistically together to target any gut microbial imbalance (dysbiosis). Our Synbiotic contains Bifidobacteria, Lactobacillus and Streptococcus.
- Bifidobacteria (longum, lactis, bifidum) help support the immune system, limit growth of pathogenic bacteria and break down lactose into nutrients the body needs.
- Lactobacillus (plantarum, rhamnosus, gasseri, casei, reutri, acidophilus) helps limit the growth of pathogenic bacteria and produces lactic acid which serves as fuel for muscles and increases the absorption of minerals.
- Streptococcus (thermophilus) is good for breaking down food, absorbing nutrients, and supporting the immune system.
Most Synbiotics contain around 5-7 different strains but we like to double the chances of benefits, that’s why ours contains 10. The more the merrier.
6. Is coffee bad for IBS?
Coffee can be a trigger for some people with IBS, as it is a gut irritant that can cause the digestive system to speed up and lead to diarrhoea or abdominal pain.
However, not everyone with IBS is sensitive to coffee, and some people may be able to tolerate it in moderation. If you have IBS and want to try coffee, it’s a good idea to start with a small amount and see how your body reacts.
7. Can IBS affect your period?
Some people report that their IBS symptoms worsen when they’re on their period. The menstrual cycle is regulated by hormones, including oestrogen and progesterone, which can affect the gastrointestinal tract. Fluctuations in these hormones can cause changes in bowel movements, leading to constipation, diarrhoea, or abdominal pain.
8. Can stress cause IBS or make symptoms worse?
‘Can stress cause IBS?’ is a common FAQ. The gut and the brain are involved in a bidirectional communication pathway called the gut-brain axis. This involves a complex network of nerve cells, hormones, and other signalling molecules that enable communication between the central nervous system (CNS) and the enteric nervous system (ENS), which is the network of nerve cells that governs the function of the gastrointestinal tract.
The gut-brain axis plays an important role in many aspects of health, including digestion, metabolism, immune function, and mental health. Signals from the gut can influence brain function, mood, and behaviour, while signals from the brain can influence gut function and the composition of the gut microbiome. Some examples of how stress can trigger or exacerbate IBS symptoms:
- Altered gut motility: stress can cause the muscles in the digestive system to contract and spasm, leading to changes in bowel movements, including diarrhoea, constipation, or a combination of both.
- Increased sensitivity to pain: stress can also increase sensitivity to pain in the digestive system, causing abdominal discomfort, cramping, or bloating.
- Changes in gut microbiota: stress can alter the balance of gut bacteria, which can affect gut motility and increase inflammation, exacerbating IBS symptoms.
- Reduced blood flow to the gut: during times of stress, blood flow is redirected away from the digestive system and towards other parts of the body, leading to reduced digestive function.
9. Are fermented foods good for IBS?
Fermented foods are foods that have undergone a process of fermentation, in which natural bacteria or yeast break down carbohydrates and sugars in the food, producing acids, gases, and alcohol.
While fermented foods are generally considered healthy and can have beneficial effects on gut health, some people may experience digestive symptoms after consuming them. The reason for this is that some individuals may be sensitive to the by-products produced during fermentation, for example histamine, which can cause symptoms such as diarrhoea and abdominal pain.
Additionally, some fermented foods, such as sauerkraut and kimchi, are high in fibre and can be difficult to digest for some people. This can lead to symptoms such as bloating, gas, and abdominal discomfort.
10. I started with symptoms of IBS after COVID. Can COVID cause IBS?
There’s been a lot of noise around ‘can covid cause IBS?’ over the last few years. Recent research suggests that COVID-19 is associated with an increased risk of long-term gastrointestinal symptoms, including post-infectious IBS, a form of IBS caused by a virus or bacteria.
COVID-19 can alter the diversity and abundance of beneficial gut bacteria, leading to increased gut permeability, gut barrier dysfunction, and gut inflammation, which can result in dysfunction of the gut-brain axis. If your symptoms started after COVID-19, it is advised to work with an IBS specialist who can help tailor your diet and lifestyle for symptom relief
Fancy a gut-friendly snack?
Gutfulness is the latest wellness launch to hit the UK market, created by Gut Health and IBS Expert, Marilia Chamon. Made in the UK with just five natural ingredients, Gutfulness is a chewy and buttery high protein peanut snack, certified low FODMAP, offering confidence and convenience to sensitive guts. Each bar contains 10g of plant-based protein and contains no artificial sweeteners, additives, preservatives or emulsifiers. Gutfulness is a nutritious and convenient snack for those that suffer with digestive symptoms, living busy everyday lives.

Shop Gutfulness bars here
Any Questions?
Have any IBS related questions not covered above? Send us an email on [email protected] and we’ll be happy to help. Alternatively, join our Facebook Gut Support group where you can openly share and speak to other people going through similar issues around IBS.
